Researchers Discover Potential Predictive Profile of Heart Disease in Fabry Patients
Written by |
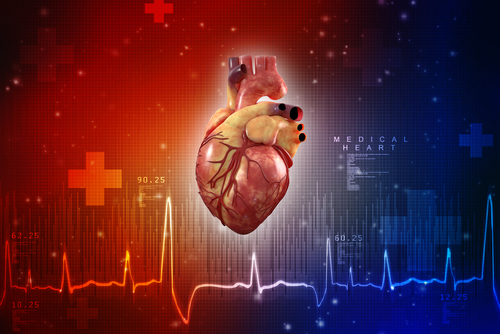
Electrical, structural, and functional changes in the heart, along with abnormal accumulation of fat molecules, may predict the development of cardiac conditions in Fabry disease patients, according to researchers.
Their study, “Cardiac Phenotype of Prehypertrophic Fabry Disease,” was published in the journal Circulation: Cardiovascular Imaging.
In Fabry disease, the accumulation of a type of fat molecule called glycosphingolipids inside cells can induce damage and cause the dysfunction of several organs, especially the kidney, heart, and brain.
Heart involvement is the leading cause of reduced life expectancy and Fabry disease-related death. Symptoms include the enlargement and thickening of the walls of the heart’s main pumping chamber (left ventricular hypertrophy, or LVH), an irregular heartbeat, heart fibrosis (scarring), and functional impairment.
LVH and heart fibrosis have been associated with an increased incidence of irregular heartbeat and sudden heart death. Once these symptoms are present, enzyme replacement therapy (ERT) becomes less effective, making the early detection of heart involvement crucial to prevent further damage.
Cardiovascular magnetic resonance is a medical imaging technology for the noninvasive assessment of the heart’s function and structure. One of its parameters, known as thermal relaxation (T1), can detect disease-associated processes, including the accumulation of fat molecules such as glycosphingolipids, identified by a low T1 measurement.
A low T1 is found in 85% of Fabry disease patients with LVH, and in 40-50% of LVH-negative patients, suggesting that the accumulation of glycosphingolipids occurs early.
Also, changes in electrocardiogram (ECG) results — a diagnostic test which monitors the electrical activity of the heart and detects heart rhythm problems — often precedes LVH.
To evaluate whether there is a predictive profile of heart disease in patients with Fabry disease, researchers analyzed the buildup of glycosphingolipids, heart rhythm problems, subtle structural and functional abnormalities, and blood biomarkers in LVH-negative Fabry disease patients.
One hundred LVH-negative Fabry disease patients (81 women and 19 men, mean age 39) have enrolled in the Fabry400 study (NCT03199001), along with 35 healthy individuals (26 women and nine men) with no history of heart disease. The trial is currently recruiting.
Among Fabry disease patients, 38 people were on ERT (median duration of seven years), and only one patient had started ERT due to heart-related symptoms.
The accumulation of glycosphingolipids, identified through low T1, was found in 59% of LVH-negative Fabry disease patients, suggesting that this process may be more common than previously reported (40-50%).
Several abnormalities in cardiac rhythm and structure were also found to be more frequent in patients with low T1. In particular, heart rate abnormalities — found in 41% of Fabry disease patients — were twice as common in these patients, and heart fibrosis was five times more likely to be present when T1 was low.
These findings suggest there is a detectable profile that predicts heart disease in Fabry patients, which consists of glycosphingolipids accumulation (low T1), irregular heart electrical activity (ECG abnormalities), and structural and functional changes.
The presence of both low T1 and ECG abnormalities were found in 31 patients, whom researchers believe may be at a higher risk of developing Fabry-associated heart disease.
According to researchers, these results support the use of low T1 to identify early heart involvement. Also, low T1 “may be a candidate starting criteria for early treatment in either practice or in clinical trials,” they wrote.