Renal Insufficiency in Fabry Patients May Lead to Cardiovascular Disease, Study Shows
Renal insufficiency in Fabry disease patients may lead to cellular events that result in cardiovascular disease, a study shows.
The study, “Serum Biomarkers of Endothelial Dysfunction in Fabry Associated Cardiomyopathy,” was published in the journal Frontiers in Cardiovascular Medicine.
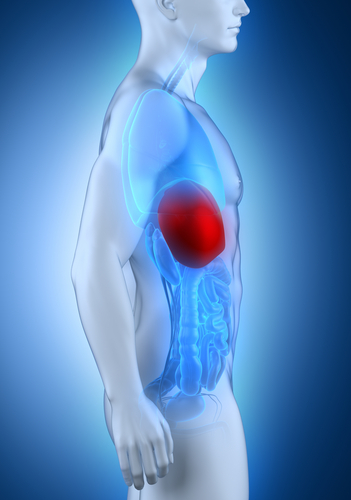
Fabry disease patients are unable to produce an enzyme called alpha-galactosidase A, which is responsible for breaking down a type of fat called globotriaosylceramide (Gb3 or GL-3).
The buildup of Gb3 in different cells of the body, including the muscles, kidneys, and heart, results in a range of symptoms, including kidney disease, stroke, heart attack, and other heart diseases.
Blood vessels are affected in Fabry patients during the early stages of the disease. Dysfunction of the endothelium — the cells that line the blood vessels — and abnormal thickening of the heart valves (myocardial fibrosis) are also observed. As such, cardiomyopathy is the leading cause of death in people with Fabry disease.
Myocardial fibrosis and subsequent cellular remodeling are caused by altered extracellular matrix (ECM) turnover, a process that involves a group of enzymes called matrix metalloproteinases (MMP). Among these is MMP-9. The ECM is a collection of molecules produced by support cells that provides structural and biochemical support to the surrounding cells, much like cement holds together a brick wall. ECM turnover is part of healthy tissue maintenance, where old proteins are degraded and new proteins formed
Increased MMP-9 levels previously have been observed in Fabry patients. Furthermore, studies have shown that these patients tend to exhibit inflammatory activity and endothelial nitric oxide synthase alterations in vascular cells. Nitric oxide synthase is a protein that produces nitric oxide from a chemical building block called L-arginine.
Nitric oxide is known to contribute to oxidative stress, a condition mainly caused by an imbalance between the activity of pro-oxidative enzymes and anti-oxidative enzymes. Oxidative stress affects endothelial and vascular function, and contributes to vascular disease.
Inhibition of nitric oxide synthase results in high levels of MMP-9, suggesting a link between oxidative stress and ECM turnover.
To better understand the role of oxidative stress and ECM turnover, researchers set out to determine the pathological mechanisms that lead to development of the disease.
Serum samples from 17 healthy controls, 15 patients with Fabry cardiomyopathy (FC) and 7 Fabry patients without FC were collected between September 2014 and December 2016.
Results revealed that MMP-9 along with another protein, called angiostatin, were significantly high in Fabry patients (regardless of whether they had FC) compared to healthy individuals. This indicates there is a higher level of ECM turnover in Fabry patients, which can drive structural changes leading to cardiovascular disease.
Symmetric Dimethylarginine (SDMA) is an amino acid — the building blocks of proteins — that has an indirect effect on nitric oxide synthase, particularly in the kidneys, and is involved in oxidative stress. SDMA concentrations were higher in patients with Fabry disease with FC than in Fabry patients without FC or the healthy controls.
SDMA concentrations were positively correlated with disease activity such as high indexed LV-mass (which indicates thickening of the myocardial wall), high sensitive Troponin T (an indicator of heart disease) and high levels of Gb3.
High SDMA levels can indicate kidney dysfunction; consequently, researchers found a significant correlation between kidney and cardiac function in Fabry patients.
“This study provides evidence for an altered ECM turnover with higher levels of MMP-9 and angiostatin in [Fabry] patients independent of an existing FC,” the researchers said.
The authors hypothesized that “accumulation of SDMA due to renal insufficiency in [Fabry disease] might contribute to the development of endothelial dysfunction and subsequently lead to FC.”