Early diagnosis, ERT prevent worse symptoms for man with Fabry
Case report details patient's successful treatment with agalsidase alfa
Written by |
Early diagnosis and a quick start to enzyme replacement therapy (ERT) with agalsidase alfa eased a patient’s Fabry disease symptoms, preventing them from getting worse for at least six months.
That’s according to a new report from China that detailed the case of a man in his 30s, who was diagnosed with Fabry after various tests and quickly started on treatment.
“Commencing ERT at an early stage may be more efficacious than [among] patients with more advanced stages of the disease,” the researchers wrote, noting that Fabry “is a progressive disorder, so early initiation of ERT has the potential to eliminate major organ damage, and yield enhanced long-term benefits.”
The diagnosis and treatment of the patient were described in “Case report: enzyme replacement therapy for Fabry disease presenting with proteinuria and ventricular septal thickening,” which was published in BMC Nephrology.
Researchers stress need for early diagnosis, quick treatment in Fabry
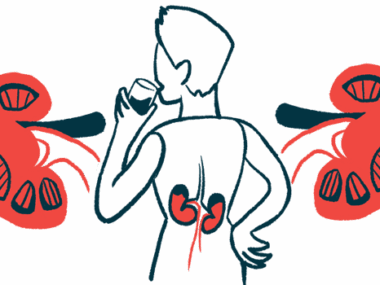
Fabry disease is caused by mutations in the GLA gene, which codes for alpha-galactosidase A, known as alpha-Gal A, an enzyme that breaks down a fatty molecule called globotriaosylceramide, or Gb3. When alpha-Gal A is faulty, Gb-3 builds up in cells, leading to symptoms — mainly in the kidneys, heart, and nervous system.
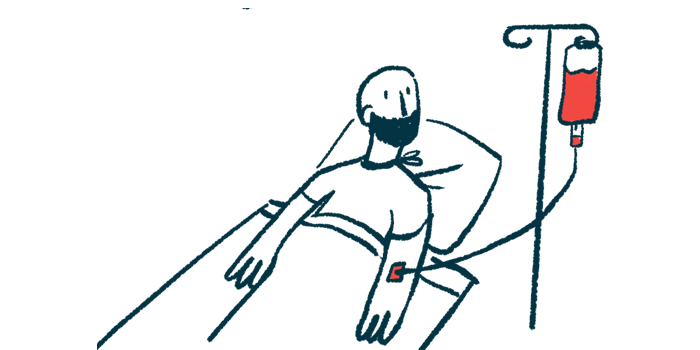
Enzyme replacement therapy, known simply as ERT, is designed to provide the body with a working version of the enzyme that’s faulty, so as to ease disease symptoms. Because Fabry symptoms become gradually worse over time, ERT should be started as early as possible in the course of the disease, ideally before any organ damage has occurred.
In this case, a 37-year-old man was admitted to the First Navy Hospital of Southern Theater Command in Zhanjiang. He was experiencing recurrent proteinuria, or excess proteins in the urine, and thickening of the heart’s ventricular septum, the wall that separates the ventricles — two lower chambers of the heart — from one another.
The man had a history of Hashimoto’s, an autoimmune disease that causes inflammation of the thyroid gland located in the neck, and preexcitation syndrome, a heart disease in which the heart’s ventricles are activated too early.
However, he had no history of reddish or dark-blue spots on the skin, known as angiokeratomas, numbness or tingling sensations in the hands or feet, blurry vision, or excessive sweating, called hyperhidrosis. All are typical symptoms of Fabry disease.
Urine tests revealed an excess of proteins and the presence of red blood cells. The kidneys appeared normal in size, but a kidney biopsy revealed the presence of foamy podocytes, a type of cells in the kidneys that wrap around blood vessels to help filter waste and fluid from the blood.
The podocytes also contained myelin bodies, known as zebra bodies, a hallmark of Gb3 buildup in cells. These findings were consistent with nephropathy, or damage to the kidneys, caused by Fabry disease.
Further testing revealed low alpha-Gal A activity in white blood cells, and high levels of Gb3. Genetic testing revealed a mutation in the GLA gene, c.902G>A (Arg301Gln), that has been linked to late-onset Fabry disease, which generally manifests after the age of 30. Based on this information, a Fabry diagnosis was made.
It is imperative to confirm a definitive diagnosis to have timely access to … appropriate management, and supportive treatment.
The man was started on an angiotensin receptor blocker — a type of medication usually used to lower blood pressure — to control proteinuria, followed by intravenous, or into-the-vein, administration of agalsidase alfa at 0.2 mg/kg of body weight every other week.
That therapy, which is not marketed in the U.S., has been approved in the European Union (EU) since 2001 and also is approved in many other countries worldwide. It is sold under the brand name Replagal.
“The patient received ERT shortly after his initial diagnosis, and both his proteinuria and ventricular septum thickness remained stable,” the researchers wrote.
Over a six-month follow-up, he remained “in good health with no clinical symptoms,” they added.
“Initiating ERT at an early age can effectively decrease the deposition of [Gb3], attenuate the progressive clinical manifestations of [Fabry disease], and provide greater long-term benefits,” the team wrote, also noting that “it is imperative to confirm a definitive diagnosis to have timely access to … appropriate management, and supportive treatment.”