Early Treatment Initiation May Prevent Lung Function Decline in Fabry Disease Patients, Study Suggests
Written by |
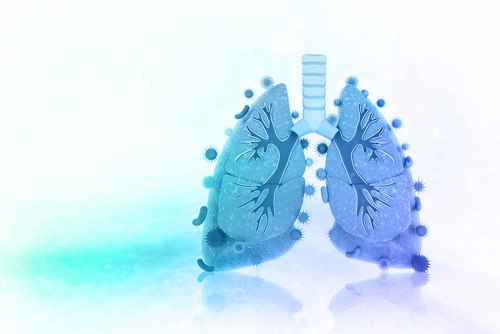
Increased levels of fat molecules characteristic of Fabry disease are linked to lung function decline over time. Progressive airflow limitation in Fabry patients can be prevented by starting treatment early with replacement enzymes, according to a recent report.
The study, “Pulmonary involvement in Fabry disease: effect of plasma globotriaosylsphingosine and time to initiation of enzyme replacement therapy,” was published in BMJ Open Respiratory Research.
Fabry disease is caused by a genetic mutation in the GAL gene, leading to absence or reduced amounts of the α-galactosidase A enzyme.
As a result, patients accumulate fat molecules called globotriaosylceramide (Gb3) and related glycosphingolipids in lysosomes of all cells in the body, including globotriaosylsphingosine (Lyso-Gb3).
While the damaging effects of Gb3 and Lyso-Gb3 on the heart, skin, kidneys, and nervous system are widely recognized, little is known about their impact on lung function.
Researchers in Zurich, Switzerland, evaluated changes in respiratory function in 53 patients with confirmed Fabry disease who were followed for a median period of 7.7 years.
Eight patients were found to have limited airflow at the beginning of the study, whereas 27 patients experienced a significant deterioration of their respiratory function over the study’s duration.
Lung function decline was measured by the ratio of FEV1/FVC, representing the proportion of a person’s vital capacity that they are able to breathe out in the first second of forced expiration (FEV1) to the full, forced vital capacity (FVC).
Men with the classical presentation of the disease (early-onset Fabry) were found to be the most affected. They had an annualized lung function decline rate of 0.048, which was 6 and 3.7 times more pronounced than that experienced by women with classical and late-onset Fabry disease.
Men with late-onset disease were found to experience smaller changes in airflow capacity, but with a tendency to slightly improve over time.
The differences between classical and late-onset patients can in part be explained by residual GAL enzyme activity in the late-onset group. This may be sufficient to help clear the lungs and prevent lung function deterioration in a shorter period of time, researchers said.
Additional analyses revealed that several factors were significantly associated with poorer respiratory outcomes in these patients. In particular, cigarette smoking and a later start of enzyme replacement therapy (ERT) were found to contribute to faster lung function decline.
In addition, higher levels of Lyso-Gb3 were found to be significantly associated with a faster deterioration of airflow capacity.
“Plasma Lyso-Gb3 is likely to be a useful predictor of pulmonary involvement in terms of early airflow limitation and might help for risk stratification and treatment decisions,” the researchers wrote.
This newly described association suggests the existence of pulmonary involvement in Fabry disease.
“There are limited data on the effect of ERT on pulmonary involvement of Fabry disease, and the optimal time for initiation of ERT is unknown,” they said. But these findings suggest that earlier treatment initiation may help stabilize respiratory decline and preserve lung function.
Researchers cautioned that additional studies are necessary to confirm these findings in larger groups of patients.