Heart, kidney transplants a success in man with late-onset Fabry
Case report details 2 surgeries 7 years apart in patient with organ damage
Written by |
A man diagnosed in his 60s with late-onset Fabry disease had an “uneventful” recovery after receiving both a heart and a kidney transplant in surgeries seven years apart, according to a new case report.
“Heart and kidney transplants can play a major role in patients with Fabry disease who develop end organ damage,” the researchers wrote. End organ damage refers to injuries that severely impair vital organs of the body to the point that the organ is close to entering into failure.
In this case, the man had “an excellent outcome” following the two transplants, the researchers noted.
“Our case report contributes to the concept that organ transplantation has a place in the management of patients with Fabry disease with end-stage organ dysfunction,” the team concluded.
The report, “A Case Report of Kidney After Heart Transplant in Patient With Fabry Disease,” was published in Transplantation Proceedings.
Symptoms of late-onset Fabry milder, but organ damage can occur
Fabry disease is caused by mutations in the GLA gene, which codes for the alpha-galactosidase A enzyme, known as Gal A, that’s necessary to break down a fatty molecule known as globotriaosylceramide or Gb3.
The mutations result in the absence of Gal A or in the production of a defective enzyme that cannot break down Gb3 as it should. As a result, the fatty molecule builds up to toxic levels in cells, causing damage to multiple tissues and organs.
In its classic form, Fabry disease first manifests in childhood or adolescence. Symptoms get progressively worse over time and can lead to serious complications such as heart and kidney failure, nerve damage, and stroke.
In people with late-onset Fabry disease, however, symptoms emerge in adulthood, generally after age 30. This form of the disease is usually milder, but most patients still will experience damage in the heart or kidneys.
Late-onset Fabry disease has a “more variable disease course, in which patients are generally less severely affected” and its “disease manifestations may be limited to a single organ, presenting in the sixth to eighth decade of life,” the researchers wrote.
[Heart and kidney problems] are the disease’s 2 most important life-threatening manifestations and can contribute to higher … mortality.
Now, researchers in Ghana and the U.S. described the case of a man with late-onset Fabry who experienced damage to both the heart and the kidneys. He had two transplants separated by about seven years, both successful.
Heart and kidney problems “are the disease’s 2 most important life-threatening manifestations and can contribute to higher … mortality,” the researchers wrote.
However they noted that “the benefit of dual organ transplantation in Fabry disease is not well established.”
Further, “patients with multiple organ involvement have a higher disease burden that can impact the quality of life and mental health, resulting in poor transplant candidacy,” they noted.
‘Excellent’ results seen in years following heart, then kidney transplant
Here, the patient — at age 56 — first showed signs of atrial fibrillation, an irregular heart rhythm that begins in the heart’s upper chambers, and a malfunctioning sinus node. The sinus node serves as the heart’s natural pacemaker.
He was implanted with an artificial pacemaker, but five years later, developed further complications. At that time, he was given a defibrillator, a device similar to a pacemaker that helps restore the heart’s rhythm.
Over time, the man’s heart muscle grew thicker, a condition called nonobstructive hypertrophic cardiomyopathy. While this did not block blood from flowing, the amount of blood the heart can hold and send to the body with each heartbeat was reduced.
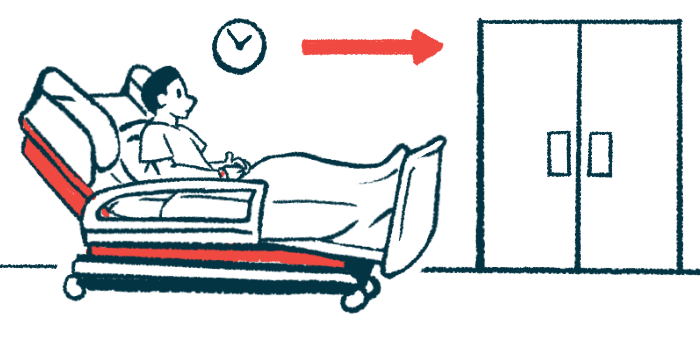
Eventually, at age 62, the man had a heart transplant. He also was put on immunosuppressants to reduce the chances that the body would reject the transplanted organ.
Testing at that time showed higher-than-normal blood levels of creatinine, a waste product normally filtered out by the kidneys, which suggested his kidneys were not be working well.
“He developed a progressive decrease in his renal [kidney] function after the heart transplant with a rising creatinine level,” the researchers wrote.
When doctors looked at a biopsy of the man’s kidneys, they found that cells appeared foamy. They also contained myelin bodies, or zebra bodies, a hallmark of Gb3 buildup in cells.
Genetic testing revealed a disease-causing mutation known as R301Q in the GLA gene, and a diagnosis of Fabry disease was made. The man’s Gal A enzyme levels were low, consistent with the diagnosis.
In retrospect, doctors deemed his heart problems were linked to Fabry disease.
“A high index of suspicion is required to diagnose Fabry disease as the initial presentation may mimic several systemic diseases,” the researchers wrote, noting “the importance of including testing for Fabry disease in the pre-transplant workup to avoid delay in management.”
The man was started on enzyme replacement therapy (ERT) to provide the missing enzyme, but his “kidney function continued to decline with worsening proteinuria while on ERT.” Proteinuria refers to high protein levels in urine.
He eventually had a kidney transplant at the age of 69, and continued to have “excellent graft function thirteen years after heart transplant and six years after kidney transplant,” the researchers wrote.
He also continued to receive ERT to prevent further Fabry-related damage. “The continuation of ERT after organ transplantation is vital in managing Fabry disease to prevent the progression of other disease-specific manifestations,” the team concluded.