Liver Transplant Did Not Restore Fabry Patient’s GLA Levels, Case Study Finds
Written by |
Transplanting the liver may not be an effective strategy to restore α-galactosidase A (GLA) levels — the deficient enzyme in Fabry disease patients — according to a case report.
The report, “Persistent Alpha-galactosidase A Deficiency following Simultaneous Liver-Kidney Transplantation in a Patient with Fabry Disease,” was published in the journal Transplantation.
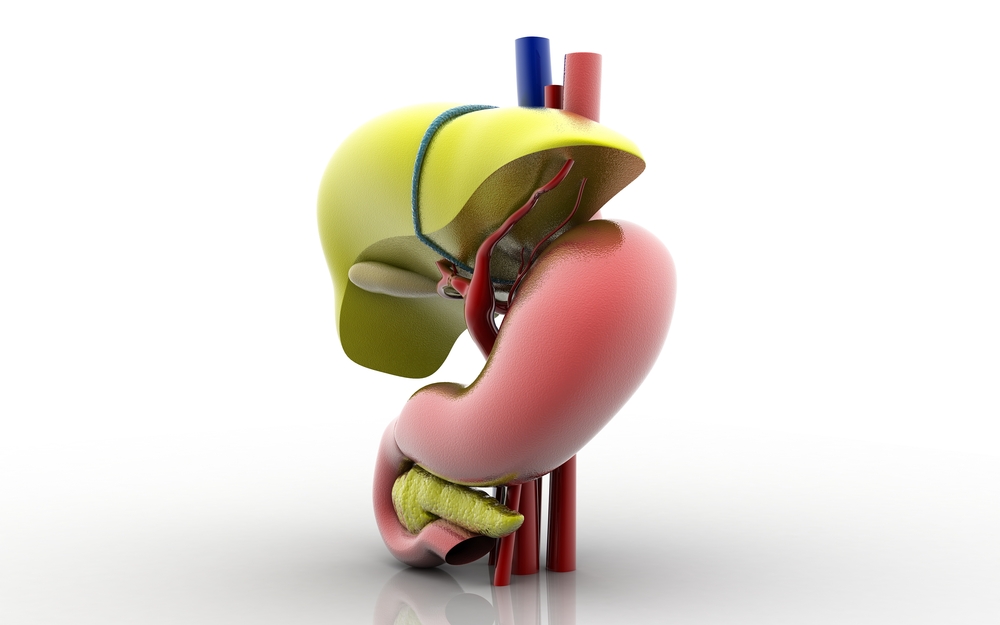
Fabry disease is a lysosomal storage disorder caused by mutations in the GLA gene, which result in absent or markedly reduced activity of the GLA enzyme. This leads to the accumulation of GLA’s major target molecules — globotriaosylceramide (Gb3) and lyso-Gb3 — in various tissues and organs, such as the heart, kidney, nervous system, eyes, and skin.
The main complications of Fabry disease are more prominent in patients older than 30, which is when kidney, heart, and/or cerebrovascular disorders — those affecting the blood vessels of the brain or brain circulation — appear.
Kidney transplant has become increasingly relevant in the management of patients with Fabry disease, as it is believed to replace not only the damaged organ, but also to restore, to some extent, the normal levels of GLA activity. However, data on this strategy are limited and somewhat contradictory, with case studies reporting disease relapse or no signs of disease recurrence years after kidney transplant.
Enzyme replacement therapy (ERT) is known to slow disease progression and relapse rate in Fabry disease patients. It is recommended after kidney transplant to reduce recurrence of Gb3 deposition and to potentially reduce disease progression of non-kidney related aspects.
Although a liver transplant also could, in theory, improve the activity levels of GLA in Fabry disease patients, the clinical benefits of this procedure are unknown. Only one study, published 30 years ago, reported improvements in disease symptoms in patients who received fetal-liver transplants, but without significant changes in GLA levels.
Researchers reported the case of a 52-year-old African-American woman with alcoholic liver disease and kidney failure associated with Fabry disease. Fabry disease diagnosis was based on low levels of GLA, the presence of a known mutation in the GLA gene, and the observation of specific damage in kidney tissue.
The patient needed a simultaneous liver and kidney transplant, and the team hypothesized the new liver could help restore GLA levels, improving Fabry disease symptoms. The 44-year-old donor was assumed not to have Fabry disease, given that his/her donated kidney was healthy.
Although GLA levels were restored to normal levels four weeks after the transplant, they subsequently decreased three and four months after surgery, along with the increase in lyso-Gb3 levels.
Researchers believe the temporary normalization of GLA levels may be due to a “short-term lysosomal enzyme [GLA] released from the transplanted organ.” However, the liver transplant was not able to induce positive long-term effects on GLA levels and Fabry disease management.
The patient started enzyme replacement therapy to restore GLA levels, and no kidney/liver problems were reported one year after transplant.