Mitochondrial TRAP1 Helps Restore Lysosome Function in Early Study
TRAP1 may be novel therapeutic target for disorders of the central nervous system
Written by |
Activating a mitochondrial protein called TRAP1 can help to improve the functionality of lysosomes, the cellular structures that are defective in Fabry disease, a new study reports.
The study, “Activation of mitochondrial TRAP1 stimulates mitochondria-lysosome crosstalk and correction of lysosomal dysfunction,” was published in iScience.
Lysosomes are the “recycling centers” of the cell, responsible for breaking down complex molecules into simpler components that can be repurposed within the cell. Fabry disease is a lysosomal storage disorder — one of more than 60 genetic conditions in which lysosomes do not work correctly, resulting in a toxic buildup of molecules inside cells.
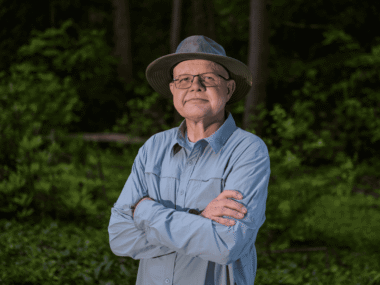
“Researchers have always looked for drugs that could recover the function of lysosomes to try to impact lysosomal storage diseases,” Juan Marugan, PhD, a study co-author from the National Center for Advancing Translational Sciences, said in a press release.
Marugan and colleagues were initially conducting screens of thousands of molecules in cell models of a lysosomal storage disorder called Niemann-Pick disease type C1 (NPC1). The team identified two molecules — referred to as ML405 and 1685 — that could limit the abnormal buildup of cholesterol and fat molecules in these cells.
The molecules showed similar effects in mouse and human cells, and in cells with various NPC1-causing mutations, including those that completely lacked the protein whose mutations cause NPC1.
“As the compounds act independently of the NPC1 protein, we speculated that the target of ML405/1685 might be a general regulator of [lysosome] function,” the researchers wrote.
ML405 treatment reduced toxic buildup of cholesterol and fats in cells
To evaluate this idea, the team tested the two molecules in cell models of other lysosomal storage disorders, including Fabry disease, Gaucher, and Pompe. While the specific lysosomal defect is different in each of these conditions, all are characterized by abnormal buildup of cholesterol and fats in cells. In all of these disease models, treatment with ML405 led to a marked reduction in this toxic buildup.
“Treatment with ML405 reduced the cholesterol storage in these cells, irrespective of the lysosomal enzyme defect, lending further support to the idea that the protein target of ML405 is a broad modulator of lysosomal function that is therapeutically effective in multiple [lysosomal storage disorders],” the researchers wrote.
Fabry disease is specifically characterized by buildup of a fatty molecule called Gb3, mainly in the kidneys and heart, leading to symptoms such as skin abnormalities, eye problems, and severe pain and tingling in the hands and feet. In a mouse model, ML405 treatment reduced Gb3 buildup in the kidneys and heart by more than 50%. The medication did not show a clear effect in NPC1 mice, though the researchers noted that this may be because it cannot get into the brain, the main organ affected in that disorder.
“Our data indicate that although the agonists are equally effective against TRAP1 in in vitro assays [in cells], they do show differences in vivo [in living animals], possibly owing to their pharmacokinetic properties,” the researchers wrote.
In a battery of biochemical tests, the researchers identified the target of ML405 and 1685 inside cells. They found that these compounds activate TRAP1, a protein that is known to be involved in the function of mitochondria — the so-called “powerhouse of the cell.” Increasing TRAP1 levels reduced cholesterol buildup in the lysosomal storage disorder cell models, similar to treatment with the compounds.
“Increasing TRAP1 activity promoted mitochondrial protein folding and facilitated the cell’s proper balance. These first-in-class molecules activate TRAP1 in the mitochondria and reduce storage in lysosomal storage diseases,” Marugan said.
“These results provided further evidence that TRAP1 is the protein target of ML405/85, albeit raising a significant question: how does a mitochondrial chaperone affect lysosome function?” the researchers wrote.
Further experimentation showed that activating TRAP1 set in motion a chain of events that led to activation of a protein called AMPK, which is known to promote lysosomal function.
“What is surprising is that TRAP1, when activated, initiates a cascade that leads to restoration of normal lysosomal function in lysosomal storage diseases,” said Yiannis Ioannou, PhD, a study co-author from the Icahn School of Medicine at Mount Sinai in New York. “Keep in mind that the defect causing each lysosomal disease is still present, so this cross-talk bypasses the genetic defect.”
This discovery may also have applications beyond lysosomal storage disorders such as, for example, in neurological conditions like Alzheimer’s or Parkinson’s disease, which are often characterized by lysosome dysfunction.
“Our data demonstrate that mitochondrial TRAP1 is a potential novel therapeutic target for multiple disorders that affect the central nervous system,” Ioannou said.