New Strategy Used in Fabry Mouse Model Holds Potential for Gene Therapy
Written by |
Using a new harmless version of an adeno-associated virus (AAV), scientists successfully delivered a human version of alpha-galactosidase A — the faulty enzyme in people with Fabry disease — to different tissues and organs, including the brain, of a mouse model of the disease.
According to the researchers, these findings indicate that a gene therapy using this new viral vector may potentially overcome the limitations of other treatments for Fabry, including their inability to reach the central nervous system (CNS; the brain and spinal cord), and tackle the neurological manifestations of the disease.
Findings were reported in the study, “Systemic treatment of Fabry disease using a novel AAV9 vector expressing α-Galactosidase A,” published in the journal Molecular Therapy Methods & Clinical Development.
Fabry is a rare genetic disorder caused by mutations in the GLA gene that normally lower the activity of alpha-galactosidase A, an enzyme responsible for breaking down a fatty molecule called globotriaosylceramide (Gb3). In the absence of functional alpha-galactosidase A, Gb3 starts to accumulate inside different tissues and organs, interfering with their normal function.
Enzyme replacement therapy (ERT), a form of treatment in which an artificial enzyme is given to patients to compensate for the faulty one, is currently the gold standard treatment for Fabry. However, ERT has some shortcomings that limits its ability to be used as a long-term treatment option for Fabry patients.
First, these artificial enzymes have a relatively short half-life — the time it takes for the levels of a compound circulating in the body to drop to half of the original amount given.
In addition, they are unable to cross the blood-brain barrier, which is the semi-permeable barrier that separates the brain from the blood circulating in the rest of the body. This means they can’t reach the brain.
Chaperone replacement therapy (CRT), a type of treatment that uses chaperones (proteins that help fold other proteins) to stabilize and partially restore the activity of faulty forms of alpha-galactosidase A, has been recently introduced to treat Fabry.
Despite being able to reach the brain, Galafold (migalastat) — an approved CRT developed by Amicus Therapeutics — is only indicated for a small group of patients carrying certain mutations.
These limitations potentially could be overcome by gene therapy, which typically uses a viral vector to deliver a functional copy of the GLA gene to cells to restore the levels and activity of alpha-galactosidase A.
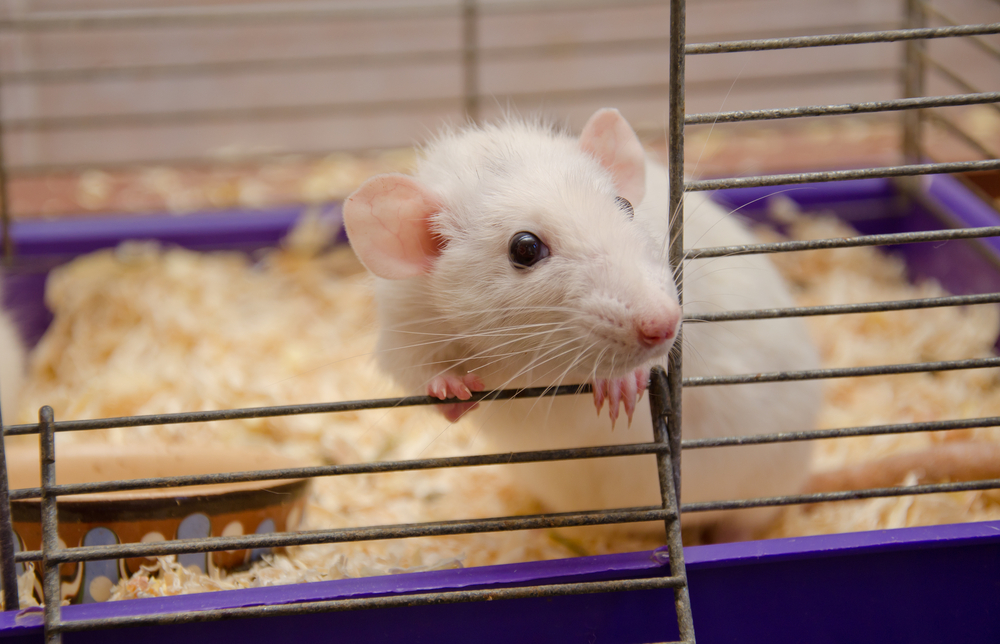
In this study, researchers at the Institute of Myology in France and their colleagues tested the effectiveness of a specific type of AAV vector, called AAV9, to deliver a DNA molecule encoding the human version of alpha-galactosidase A to a mouse model of Fabry.
They first administered a single dose of the gene therapy (scAAV9-PGK-GLA) intravenously, or directly into the vein, to newborn mice that had been genetically engineered to be unable to produce alpha-galactosidase A.
Three and five months later, they measured the enzyme’s activity in different organs, including the brain, spinal cord, liver, heart, and kidneys. The human enzyme was detected in all tissues at both time points, although its activity was higher five months after receiving treatment.
Treatment also lowered Gb3 levels in some of the analyzed tissues at both time points.
They then administered a single dose of the gene therapy to adult animals of both sexes before and after they started showing the first symptoms of the disease.
The human enzyme was found to be active in the brain, heart, liver, and kidneys of all treated animals, regardless of whether they had already shown the first signs of the disease. They also discovered that alpha-galactosidase A remained active and prevented the buildup of fatty molecules in several tissues up to five months after treatment.
Additional analyses also showed that nine of the 32 treated animals started producing antibodies against the human enzyme. However, these antibodies did not have a significant impact on the enzyme’s activity in the different tissues analyzed.
“These results demonstrate that scAAV9-PGK-GLA can drive widespread and sustained expression [activity] of [alpha]-Galactosidase A, cross the blood brain barrier after systemic delivery and reduce pathological [disease] signs of Fabry Disease mouse model,” the researchers wrote.
“Given that the standard of care, ERT, does not reach the CNS and chaperon therapy is indicated for a restricted group of patients, the proposed gene therapy vector represents a promising preclinical therapeutic candidate for [Fabry disease], which overcomes most of the limitations of currently used approaches,” they concluded.