Rare double mutations linked to case of cardiac Fabry in Japan
Patient in case study was treated with chaperone therapy Galafold
Written by |

A rare pair of mutations were identified as the likely cause of Fabry disease for a young man with cardiac involvement in Japan who was successfully treated with Galafold (migalastat).
While the clinical significance of the two mutations has not been well established, researchers believe their combined effects were the cause of disease.
The case report, “A novel double GLA gene mutation of W24R and N419D in a patient with cardiac Fabry disease,” was published in Molecular Genetics and Metabolism Reports.
Fabry disease is a rare genetic condition caused by mutations in the GLA gene resulting in the toxic cellular accumulation of certain fatty molecules due to a lack of the alpha-galactosidase A (Gal A) enzyme. Damage can be observed in many organs, especially the heart, kidneys, and brain.
The condition is inherited in an X-linked dominant manner, meaning that a person needs to have only a single disease-causing mutation on the GLA gene that resides on the X chromosome to exhibit symptoms. Because men have only one X chromosome, the consequences of the mutation are typically more severe than in women, who may have one one faulty copy of GLA and another healthy one.
2 distinct mutations of the GLA gene detected
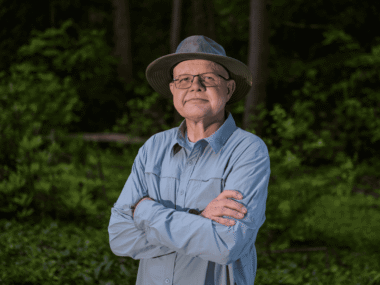
Now, the researchers reported a familial case of Fabry disease in which a young man had two distinct mutations on his GLA gene. He was admitted to the hospital due to heart failure.
The man, in his 20s, was severely obese, but otherwise did not have health issues.
A battery of heart imaging tests led to a diagnosis of idiopathic dilated cardiomyopathy, when the heart muscle is weakened and enlarged for an unknown reason.
He was discharged after a month of treatment in the hospital, and continued treatment for heart failure. The man failed to lose weight, but his heart gradually began to improve.
During the course of his treatment, the doctors began to suspect the man had left ventricular hypertrophy, a thickened wall of the heart’s main pumping chamber. In light of the fact that heart problems ran on his mother’s side of the family, the researchers began to search for the underlying cause of his heart failure.
They identified significantly reduced Gal A activity in the man’s white blood cells, leading to a Fabry diagnosis.
Fatty waste products known to accumulate in Fabry, including globotriaosylceramide (Gb3) and lyso-Gb3, were also elevated in the man’s blood and urine.
Genetic analyses revealed two distinct mutations in different areas of the GLA gene. While double mutations have been reported in Fabry before, these ones “are rare and thus represent a novelty,” the researchers noted.
Lab studies indicate that each mutation — called W24R and N419D — can lead to reduced Gal A activity, but their clinical significance in patients hadn’t yet been determined.
“It is unknown whether these mutations each or in combination exert pathogenicity [cause disease],” the researchers wrote.
Nevertheless, the scientists speculated that the combination “might only synergistically attain or potentiate the pathogenicity of [Fabry].”
In other words, while each mutation alone might not have a strong effect, together, they drive a sufficient Gal A reduction to cause Fabry symptoms.
Galafold prescribed after enzyme replacement therapy discontinued
The man was started on enzyme replacement therapy, which was discontinued after 1.5 years due to feasibility issues related to the need for frequent into-the-vein infusions.
He was then started on oral Galafold, which the man had been on for three years without any issues at the time of the report. Lyso-Gb3 levels continued to fall.
A type of chaperone therapy, Galafold binds to unstable or dysfunctional versions of Gal A and stabilizes them. It only works for certain types of mutations. Both W24R and N419D appear to be amenable to Galafold, the team noted.
After the diagnosis, the man’s parents were referred for Fabry screening. While both parents were healthy, his mother had several male siblings who had died from an unknown disease associated with cardiac problems and sudden death.
Genetic testing revealed she had the same mutations as her son, but with normal Gal A activity and no organ damage. She had some minor elevations in lyso-Gb3, leading to a diagnosis of least manifest Fabry disease. The rest of her family was not tested.