Heart failure in woman with Fabry disease treated with transplant
Report shows Fabry-related heart failure can be managed with heart transplant
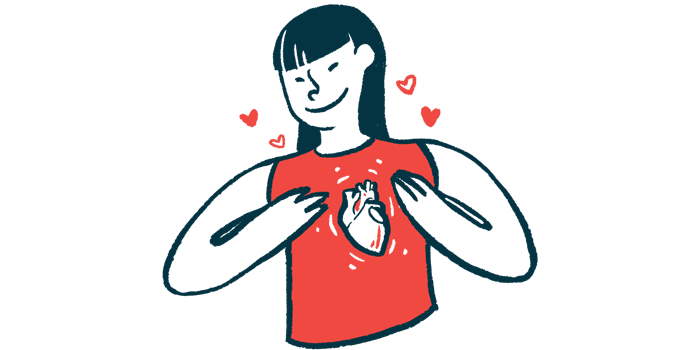
A woman with heart failure due to late-onset Fabry disease received a heart transplant in combination with immunosuppressants and Fabrazyme (agalsidase-beta) to resolve her cardiac symptoms, which didn’t recur after the transplant.
“Although the risk of disease recurrence in the transplanted organ appears to be relatively low, this observation requires further investigation with extended follow-up and a larger study sample,” wrote researchers in Poland. Their report, “Enzyme Replacement and Immunosuppression in Heart Transplant Recipients with Fabry Cardiomyopathy: A 7-Year Case Study,” was published in the American Journal of Case Reports.
Fabry disease is a storage disease caused by genetic mutations that lead to a deficiency of the enzyme alpha-galactosidase A (alpha-Gal A). Without it, fatty molecules called glycosphingolipids build up to toxic levels in cells, causing symptoms and organ damage.
Unlike classic Fabry disease, which manifests during childhood or adolescence, symptoms of late-onset Fabry disease don’t start until adulthood, after age 30. They usually involve a major organ, such as the heart, as was the case of a 38-year-old woman with heart failure.
Diagnosis of Fabry disease
During a routine check for shortness of breath, an X-ray showed she had an enlarged heart. An echocardiogram, or ultrasound of the heart, revealed thickening of the heart muscle walls and the left ventricle, one of the heart’s bottom chambers, was enlarged.
The woman was diagnosed with hypertrophic cardiomyopathy, where thickening of the heart muscles makes it difficult for it to pump blood, and was started on beta-blockers, which work mainly by slowing down the heart.
Another routine check six years later suggested a storage disease as the cause of her hypertrophic cardiomyopathy. An electrocardiogram, which records the electrical activity of the heart, showed bradycardia (an abnormally slow heart) and deep inverted T-waves, which can be a sign of heart damage.
Further testing revealed high levels of lyso-Gb3, a type of glycosphingolipid that builds up in Fabry disease. Genetic testing identified three different mutations in the gene that codes for alpha-Gal A, leading to a diagnosis of Fabry disease.
“The patient was the first one diagnosed with [Fabry disease] in her family,” the researchers wrote. However, genetic screening of family members showed her mother, brother, two sisters, son, and a niece also carried Fabry-causing mutations.
“At the time of diagnosis, enzyme replacement therapy (ERT) was not available in Poland, so the patient received standard conservative treatment with beta-blockers and was scheduled for regular check-up visits,” the researchers wrote. ERT works by supplying the body with the missing enzyme.
Despite being on beta-blockers, the woman’s heart failure worsened over two years, resulting in a heart transplant. Aside from a small blood clot in the neck and some temporary kidney problems, which likely resulted from the surgery or the use of immunosuppressants, the woman recovered well and her symptoms eased.
Receiving ERT
About four years later, an examination showed the woman was eligible for ERT with Sanofi’s Fabrazyme. She was found to have longstanding symptoms of Fabry, such as nerve pain, lack of sweating, and skin spots, which hadn’t been linked to the disease before. A brain scan showed lesions and small strokes, common in a storage disease like Fabry.
Fabrazyme is given as an infusion into the bloodstream every other week. The first one lasted about 3.5 hours without complications, allowing subsequent infusions to be shortened by about half. Since then, she has received more than 100 doses, continuing ERT for more than 50 months, or about four years.
A biopsy to remove a piece of heart tissue five years after the transplant showed no buildup of glycosphingolipids. Regular echocardiograms showed healthy heart function and muscle walls of normal thickness. Since starting ERT, lyso-Gb3 levels have steadily decreased.
The course of ERT was complicated for a time due to a viral infection that was treated with the antiviral ganciclovir. While the immunosuppressive therapy may have weakened the woman’s immune system and increased the risk for infection, she was still on an immunosuppressant regimen with tacrolimus, mycophenolate mofetil, ramipril, lacidipine, atorvastatin, acetylsalicylic acid, and pantoprazole at the time of the report and no interactions between these immunosuppressants and ERT were seen.
The case of this woman, who was followed for six years after receiving a heart transplant, suggests that “severe heart failure not responding to medical therapy in patients with [Fabry disease] can be managed effectively with [heart] transplantation,” the researchers wrote.