How I work to prevent infection in life post-transplant
It's crucial I take every precaution to protect my weakened immune system
I haven’t read any medical literature indicating that Fabry disease weakens the immune system, but most post-transplant medications do. Many people with Fabry have organ failure and thus need kidney or heart transplants.
The antirejection medications we must take for the rest of our lives weaken our immune systems as a way to help our body accept the transplanted organs, instead of attacking them as foreign objects. While these medications help ensure the transplanted organ’s success, they also come with lifestyle changes and lifelong restrictions. Immunosuppressants not only make us more susceptible to infections, but cause any infections to be more severe and last longer because our body’s ability to fight them is reduced.
Since my heart transplant in September 2020, even minor infections — ones that would’ve resolved on their own or were easily treated at home — usually send me to the hospital for a week of strong, intravenous antibiotic treatment. It’s scary to know that any infection can quickly get out of control and endanger my life.
With each new infection, it takes a few days for blood and urine cultures to grow, after which my providers can identify the specific strain of bacteria and determine the most effective treatment. Initially, I usually start a broad-spectrum antibiotic and hope it helps while I wait to find out about the specific bacterial culprit and the best medication to fight it.
Given the current health concerns from COVID-19, respiratory syncytial virus (RSV), the annual flu surge, and potential exposure to infectious people, transplant recipients must take extra precautions to protect ourselves. Because of my weakened immune system, I haven’t flown in an airplane or been to the theater in years. I rarely eat indoors at restaurants, though outdoor dining is possible, depending on the weather. I’ve missed many important events to lessen my risk of getting sick. Although I’m relatively healthy, I feel more fragile than ever given the risk looming over me.
Steps I take to stay healthy
Following is my personal list of dos and don’ts, which includes my transplant physician’s rules as well as general COVID-19 precautions. These precautions decrease my risk of getting an infection my body can’t fight on its own, and they enable me to build up my immune system as much as possible.
- Take my transplant and other medications daily as prescribed.
- Avoid unpasteurized foods and drinks.
- Avoid processed foods.
- Avoid raw and undercooked foods.
- Drink bottled water. (Our home’s water well is susceptible to germs.)
- Avoid contact with soil.
- Avoid too much exposure to direct sunlight to minimize my increased cancer risk from my antirejection medications.
- Keep up with vaccinations for COVID-19, the flu, RSV, etc.
- Wash my hands frequently and use hand sanitizer as needed.
- Maintain skin to avoid dryness and cracks where bacteria can enter.
- Wear a mask at indoor events and around groups of people.
- Maintain a healthy immune system by:
- Eating well
- Being physically active
- Maintaining a healthy weight
- Getting enough sleep
- Not smoking
- Avoiding too much alcohol.
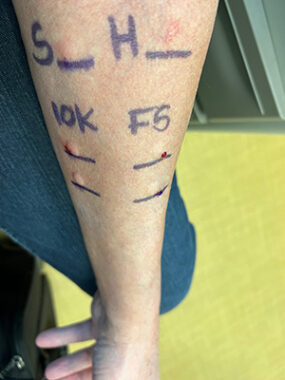
Jerry undergoes allergy testing for penicillin. (Courtesy of Jerry Walter)
Even though vaccinations are generally recommended for people with weakened immune systems, we usually don’t have as robust of an antibody response compared with the general population. For context, after my COVID-19 vaccinations, I developed a small antibody response, indicating I had some protection. However, the response of my wife, Angela, was 10 times greater. I’m at a higher risk of a poor COVID-19 outcome.
An additional step I took to increase my success in fighting infections is to verify whether I’m allergic to penicillin. My doctors have wanted to treat me with it, but when I was a child, my mother told me I was allergic to the medication. For more than 60 years, I repeated what my mother had told me. But when I finally had an allergy test in December, I learned I’m not allergic to penicillin after all. I’ll now have more treatment options when fighting future infections.
I hope my experiences help other people understand life with a transplanted organ. Like most people, my life looks different since the pandemic. Life after heart transplant is even more complicated, but better overall. Still, I have a good life full of possibilities, and I look forward to completing my bucket list.
Note: Fabry Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Fabry Disease News or its parent company, Bionews, and are intended to spark discussion about issues pertaining to Fabry disease.






Leave a comment
Fill in the required fields to post. Your email address will not be published.