PRX-102 Leads to Improvement in Fabry Patients, Phase 1/2 Data Suggest
crystal light/Shutterstock
PRX-102 (pegunigalsidase alfa), Protalix BioTherapeutics’ investigational enzyme replacement therapy, led to clinical improvements in adults with Fabry disease, according to data from two Phase 1/2 trials.
The therapy lowered both kidney globotriaosylceramide (Gb3) inclusions and blood levels of Gb3, showing that it reaches affected tissues, and further confirming its potential to lessen disease burden.
The findings were presented in a scientific poster, “Pegunigalsidase alfa, PEGylated α-Galactosidase-A enzyme in development for the treatment of Fabry disease, shows correlation between renal Gb3 inclusion clearance and reduction of plasma Lyso-Gb3,” at the WORLDSymposium 2020, held Feb. 10-13 in Orlando, Florida.
Fabry disease is characterized by the lack of alpha-galactosidase A, an enzyme responsible for breaking down a fat molecule called globotriaosylceramide (Gb3 or Gl-3), which can lead to problems in several organs and tissues, including the heart, brain, and kidney.
PRX-102 replenishes patients’ alpha-galactosidase A levels. The lab-made enzyme, developed with Protalix’s plant-based ProCellEx platform, is delivered via an infusion to the bloodstream, and aims to reduce the number of required enzyme infusions to once a month. Existing enzyme replacement therapies need to be administered every two weeks.
Two Phase 1/2 trials (NCT01678898 and NCT01769001) evaluated the safety, effectiveness and pharmacokinetics (how a drug works within the body) of PRX-102, administered intravenously every other week in adult, symptomatic, treatment-naive Fabry patients.
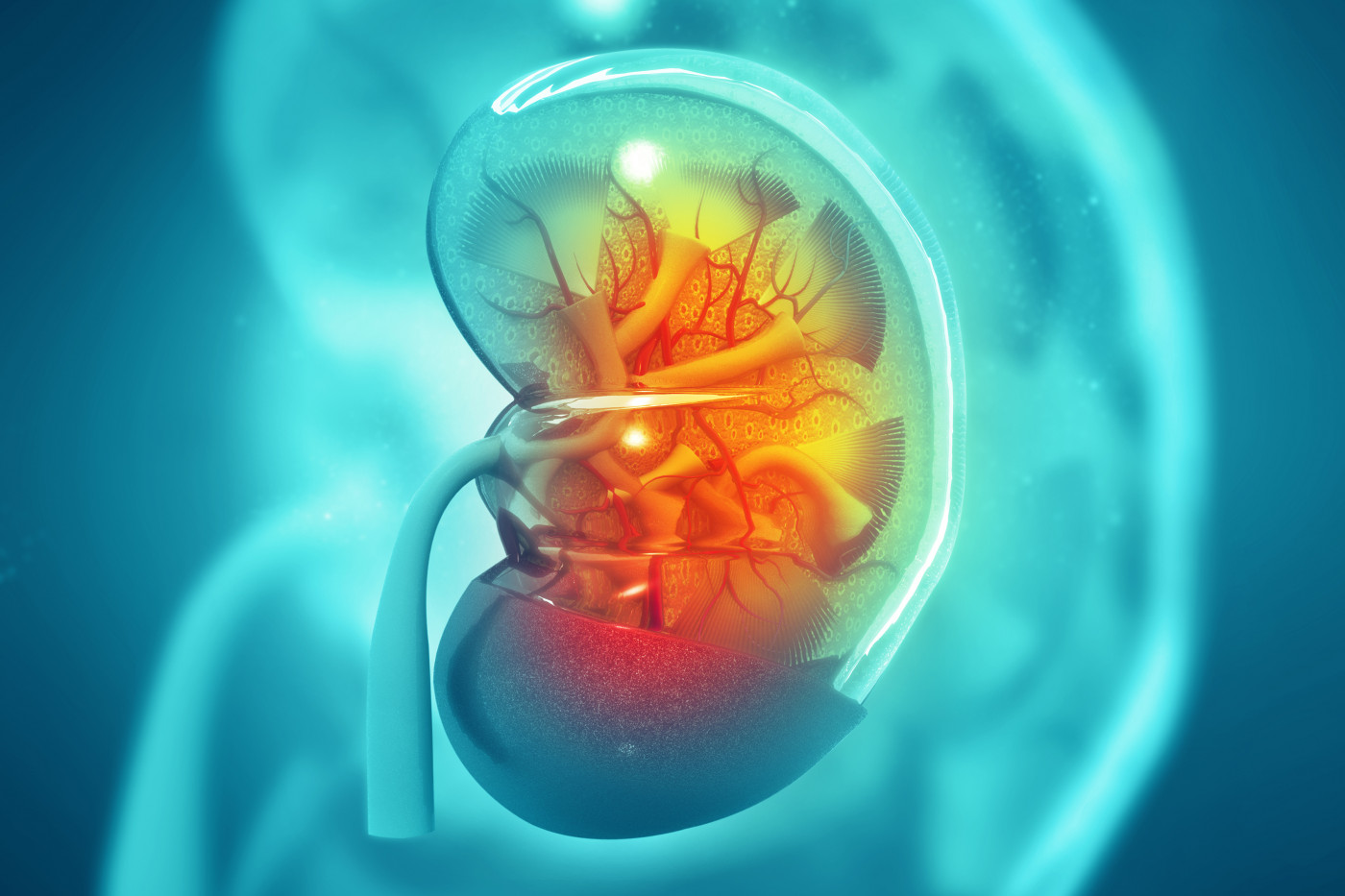
The researchers said they assessed the histological (tissue) Gb3 burden in renal peritubular capillaries (PTCs), as lowering this “is considered an appropriate and objective surrogate endpoint likely to predict clinical benefit of treatment in Fabry disease.”
PTCs are very small blood vessels in the nephron, the functional unit of the kidney that allows the blood filtration of substances to be eliminated in the urine.
Researchers examined patients’ renal biopsies and used the Barisoni Lipid Inclusion Scoring System (BLISS) to quantitatively determine Gb3 inclusions in the kidney, at baseline, and after six months of treatment. In short, this method consists of counting the GB3 inclusions per PTC, with a decrease in this score indicating clinical improvement.
Sixteen patients, in three different dose groups (0.2, 1.0 and 2.0 mg/kg), completed 12 months of treatment. Of those, 14 had renal biopsies available. Plasma Gb3 (Lyso-Gb3), a breakdown product of Gb3 and a specific biomarker for Fabry disease, was assessed for all patients.
The mean BLISS score was 4.3 at the study’s beginning, indicative of significant renal involvement, and had fallen to 0.8 after six months of treatment, a mean 67.8% drop. In the 1.0 mg/kg group, the drop was 86.5%.
Of the total biopsies available, 78.6% of patients had lowered their BLISS scores by 50% or more.
Plasma Lyso-Gb3 levels showed a significant drop after six, 12, and 24 months of treatment. There was a high correlation between the decline in the the levels of plasma Lyso-Gb3 and the reduction in kidney Gb3 inclusions, further supporting the potential effectiveness of PRX-102.
Protalix and Chiesi Farmaceutici in February announced the start of a pediatric study plan (iPSP) to test PRX-102 in children with Fabry disease.
The investigational therapy, which has been granted fast track designation as a potential treatment for Fabry disease, is also being investigated in two Phase 3 clinical trials (NCT03018730 and NCT02795676).