ST-920 Gene Therapy Found Safe, Effective in Mouse Model; Supports First-In-Human Trial
Written by |
A single administration of the experimental gene therapy ST-920 in a Fabry disease mouse model safely and effectively increased the levels of the alpha-GalA enzyme — which is lacking in people with the genetic disorder — in the liver, heart, and kidneys, a series of preclinical trials demonstrated.
These findings supported ST-920’s first-in-human Phase 1/2 clinical trial (NCT04046224), which is testing the efficacy and safety of increasing doses of the therapy in about 30 men with Fabry disease in the U.S.
The trial is currently recruiting participants in five states. Enrollment information can be found here.
The results of the preclinical trials were published in the journal Methods & Clinical Development, in a study titled “AAV2/6 Gene Therapy in a Murine Model of Fabry Disease Results in Supraphysiological Enzyme Activity and Effective Substrate Reduction.”
Fabry disease is caused by mutations in the GLA gene, which carries the instructions for an enzyme called alpha-GalA. These mutations lead to the accumulation of fatty molecules known as Gb3 and lyso-Gb3 inside cells. That buildup can cause a wide range of symptoms, including life-threatening ones such as heart attack, stroke, and kidney disease.
Enzyme replacement therapy is a current treatment, but it requires regular lifelong infusions. Chaperone therapy, another form of treatment, helps some Fabry patients with specific mutations but not all of those with the disorder can benefit.
ST-920, an experimental gene therapy developed by Sangamo Therapeutics, aims to provide patients with a fully functioning version of the GLA gene to the liver, which would release alpha-GalA into the bloodstream.
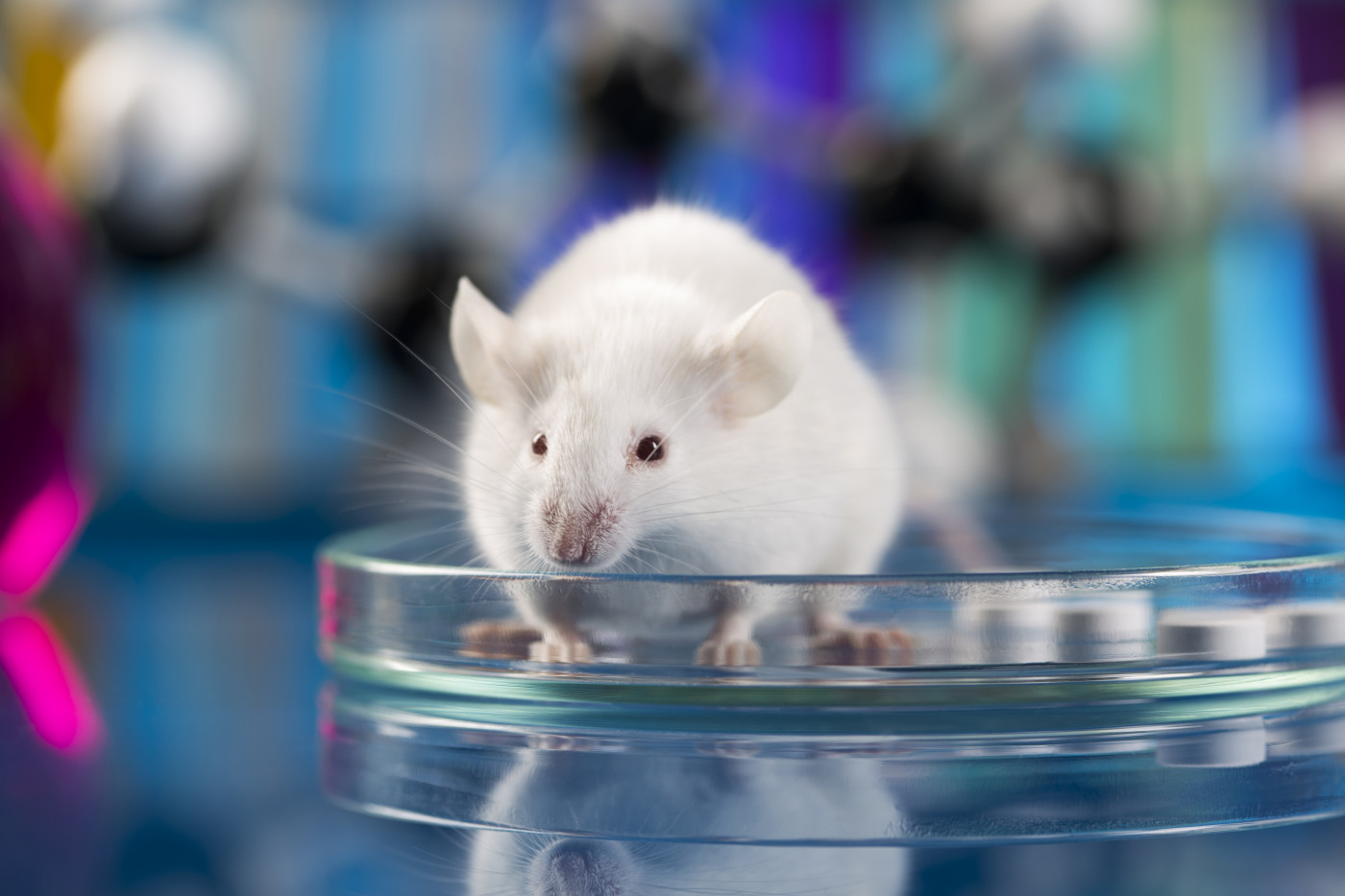
In developing ST-920 for use in clinical trials, scientists at Sangamo, in collaboration with investigators at the Icahn School of Medicine at Mount Sinai, in New York, conducted a series of preclinical trials. Those trials tested the delivery of the GLA gene using a harmless adeno-associated virus (AAV) vector into a Fabry mouse model that lacks the GLA gene.
The initial proof of concept was established in a six-month, dose-finding study in which Fabry mice, along with normal control (healthy) mice, were treated intravenously (into the vein) at different doses. After six months, dose-dependent increases in GLA DNA and alpha-GalA enzyme in the liver were observed in the treated mice, but not in the untreated or control mice.
Regularly collected blood samples showed dose-dependent increases in alpha-GalA enzyme activity over time, which were sustained for the study duration. After six months, the alpha-GalA enzyme levels were 26-fold higher in the bloodstream of mice treated at the highest dose compared with healthy mice.
The concentrations of Gb3 and Lyso-Gb3 were measured in the heart and kidney — the two main sites affected in Fabry disease. In heart tissue, Lyso-Gb3 concentrations were normalized, and Gb3 levels were reduced by more than 80% compared with untreated Fabry mice. Likewise, in the kidneys, both Gb3 and Lyso-Gb3 levels were reduced more than 80% in mice treated at the highest dose.
A three-month pharmacology and toxicology study tested a version of the treatment produced by a clinical-scale manufacturing process, called ST-920PC, using a single intravenous administration into Fabry mice.
Dose-dependent increases in alpha-GalA enzyme activity were found one week after injection and were sustained over the three months in all dose groups.
After 85 days post-treatment, the average alpha-GalA activity in blood was 408 times higher in mice treated at the highest dose compared with normal mice. Further, at the highest dose, the liver’s alpha-GalA activity increased up to 1,400-fold, and about 31-fold higher in heart tissue, and 5-fold higher in kidneys than normal mice.
Fabry mice treated at a high dose had undetectable levels of Lyso-Gb3 in the blood and all tissues analyzed, including the liver, heart, and kidney. These animals also had less than 10% of Gb3 remaining in plasma and all tissues compared with untreated Fabry mice.
Finally, the experimental ST-920PC vector was optimized to further enhance its potency — now called ST-920 — and the effectiveness of the two vectors was compared in normal mice.
Dose-dependent increases in blood alpha-GalA activity were detected eight days after injection. After 29-days post-treatment, the average alpha-GalA activity levels were 4,335-fold higher at the highest dose compared with untreated mice. This represented a sevenfold improvement of the ST-920 vector over ST-920PC.
ST-920 was well tolerated, with no observed adverse effects at the highest dose tested and no apparent clinical signs of toxicity.
“The highly optimized final lead vector, ST-920, resulted in the highest plasma and tissue transgene expression and demonstrated a good safety profile in Fabry and wild-type mice,” the researchers wrote, adding that these preclinical studies support the development of ST-920 in human clinical trials.