Experimental treatments for Fabry disease
Last updated Feb. 13, 2025, by Lindsey Shapiro, PhD

Several experimental approaches are being developed to potentially treat people with Fabry disease, a rare disease caused by genetic mutations in the GLA gene.
These mutations lead to a missing or deficient alpha-galactosidase A (alpha-Gal A) enzyme, which is crucial for breaking down certain fatty molecules, particularly globotriaosylceramide (Gb3), within specific cellular structures called lysosomes.
Without sufficient alpha-Gal A, Gb3 accumulates inside cells to toxic levels, leading to organ damage and other disease symptoms.
Although approved treatments for Fabry disease can help to slow the progression of organ damage and ease patients’ symptoms, the condition currently has no cure. Scientists are working to identify and develop new and potentially more effective therapeutic approaches.
Several classes of experimental therapies are being developed or further refined for Fabry, each addressing the disease’s faulty processes at different levels. The most advanced of these approaches include:
- enzyme replacement therapy, which temporarily provides a functional alpha-Gal A enzyme to patients
- gene therapy, which targets the GLA gene directly
- substrate reduction therapy, which aims to reduce Gb3 production.
Enzyme replacement therapy
Enzyme replacement therapy (ERT), the main approved treatment approach for Fabry, provides patients with a working version of the alpha-Gal A enzyme to temporarily replace their missing or defective enzyme. This is expected to reduce the toxic accumulation of Gb3 and other fatty molecules, slowing or preventing the progressive organ damage that characterizes the disease.
Two enzyme replacement therapies, Fabrazyme (agalsidase beta) and Elfabrio (pegunigalsidase alfa), are approved to treat Fabry disease in the U.S. Agalsidase alfa, another ERT, is available in many countries worldwide under the brand name Replagal, but it has not been approved for use by the U.S. Food and Drug Administration (FDA).
Agalsidase alfa
Agalsidase alfa is a concentrated, man-made form of alpha-Gal A that’s produced in the lab by genetically engineering human cells to have a more active GLA gene.
The therapy’s safety and efficacy were evaluated in several clinical trials involving both children and adults, where it was found to stabilize cardiac and kidney function, while lowering Gb3 levels.
Agalsidase alfa has been approved for Fabry patients in the European Union for more than two decades, where it is administered as an intravenous, or into-the-vein, infusion every two weeks. This ERT is unlikely to be approved to treat Fabry in the U.S., however, as its developer withdrew a marketing application to the FDA in 2012.
Gene therapy
Gene therapy is an approach that involves modifying a person’s genetic material to treat or prevent disease. In the context of Fabry disease, gene therapy aims to provide patients with a functional version of the GLA gene, enabling their cells to continuously produce a working version of alpha-Gal A.
By directly addressing the genetic defects underlying Fabry disease, gene therapies hold promise as a one-time treatment that allows patients to produce sufficient amounts of alpha-Gal A for the rest of their lives. As such, it could free patients from a need for lifelong therapy and serve as a potential cure for the disease.
A few gene therapies are being tested for Fabry in early clinical trials.
Isaralgagene civaparvovec
Isaralgagene civaparvovec (ST-920), being developed by Sangamo Therapeutics, is designed to deliver a healthy version of the GLA gene to liver cells. The goal is to enable them to produce functioning alpha-Gal A on their own, reducing the abnormal accumulation of Gb3 and slowing or stopping disease progression.
The investigational therapy, intended to be administered as a one-time intravenous infusion, is packaged inside a modified viral carrier that targets liver cells more specifically. Because isaralgagene civaparvovec is not expected to trigger an immune response that compromises its efficacy, it does not require pretreatment with steroids or other medicines to suppress such immune responses.
The Phase 1/2 STAAR clinical trial (NCT04046224) is evaluating varying doses of isaralgagene civaparvovec in about 34 adults with Fabry disease. Interim findings show isaralgagene civaparvovec to be well tolerated, with increased alpha-Gal A levels being sustained above the normal range for up to three years after treatment.
Most patients who were using an ERT at the time of isaralgagene civaparvovec administration were able to stop this treatment, with their alpha-Gal A levels remaining within or above normal levels.
Sangamo is planning to open a Phase 3 study of its the potential gene therapy for Fabry disease, and its data may be sufficient to support a regulatory application.
4D-310
4D-310 is an experimental gene therapy being developed by 4D Molecular Therapeutics. The therapy is being investigated in two Phase 1/2 clinical trials, one taking place in the U.S. (NCT04519749) and the other in Taiwan and Australia (NCT05629559). Administered as a single infusion into the bloodstream, this gene therapy uses a harmless viral vector to deliver a healthy copy of the GLA gene directly to heart muscle cells, which is expected to ease or improve the cardiac symptoms of Fabry disease.
AMT-191
AMT-191, an experimental gene therapy being developed by uniQure, is being investigated in a Phase 1/2 clinical trial (NCT06270316) in up to 12 men with Fabry disease. This potential one-time gene therapy is designed to deliver a working version of the GLA gene directly to liver cells, also using a harmless viral carrier.
Substrate reduction therapy
Substrate reduction therapy (SRT) is a treatment strategy, used in many lysosomal storage disorders, that aims to lower the production of the waste molecules, such as Gb3, that toxically accumulate inside cells.
In contrast with most approved and experimental therapies for Fabry, which focus on increasing alpha-Gal A enzyme activity to boost the breakdown of Gb3 and other fatty molecules, SRT approaches aim to prevent those molecules from being produced in the first place. This also is expected to reduce their toxic buildup to slow organ damage.
SRTs currently in clinical development for Fabry include venglustat, lucerastat, and AL01211. All are designed to block an enzyme called glucosylceramide synthase, which is needed to make Gb3 and related fatty molecules.
Venglustat
Venglustat is being developed by Sanofi as a potential SRT for Fabry disease and other conditions. The therapy inhibits glucosylceramide synthase, which is expected to lower Gb3 levels and ease Fabry symptoms even in the absence of sufficient alpha-Gal A.
A Phase 2a clinical trial (NCT02228460) tested venglustat, given as once-daily oral capsules for six months, in 11 men with Fabry disease. Participants then were invited to continue treatment for up to 2.5 more years in the trial’s extension study (NCT02489344).
While the treatment was considered reasonably safe, the trial failed to meet its primary goal of significantly reducing Gb3 accumulation in skin cells after six months of treatment. However, most of the patients treated for three years in the extension trial saw a reduction in Gb3 levels and showed no signs of clinical disease progression in the kidneys, heart, brain or nervous system.
Venglustat now is being investigated in two Phase 3 clinical trials — PERIDOT (NCT05206773) and CARAT (NCT05280548) — to assess its affects on abdominal and neuropathic (nerve) pain and left ventricular hypertrophy, a type of heart disease seen in many Fabry patients.
Lucerastat
Lucerastat, being developed by Idorsia, also aims to lessen the toxic accumulation of Gb3 by inhibiting glucosylceramide synthase.
Data from a Phase 1 clinical trial (NCT02930655) in adults with Fabry disease supported the therapy, given orally twice a day in addition to standard ERT treatment, as safe and well tolerated. Significantly lower blood levels of Gb3 compared with ERT alone also were seen, suggesting treatment efficacy.
A nearly 50% reduction in Gb3 blood levels after six months of treatment also was observed in the MODIFY Phase 3 trial (NCT03425539), which involved 118 adults who were not receiving ERT. But this trial failed to meet its main goal of reducing neuropathic pain.
Still, up to two years of treatment in MODIFY and its open-label extension study (NCT03737214) resulted in slower declines in kidney function and improvements in measures of cardiac health in some patients. That extension study is continuing, with those enrolled being treated for up to four years and monitored for long-term outcomes.
AL1211
AL1211, being developed by AceLink Therapeutics, is a SRT that’s reported to be more potent and better at targeting tissues affected in Fabry than other inhibitors of the glucosylceramide synthase enzyme. The therapy also is designed to have a low ability to enter the brain, which is expected to maximize its effects on targeted organs while minimizing side effects on the brain.
Data from a Phase 1 trial (NCT04908462) in healthy volunteers indicated that the therapy reduced levels of Gb3 and related fatty molecules as designed, and no serious side effects were reported.
AceLink now is sponsoring a Phase 2 clinical trial (NCT06114329) that aims to test the therapy’s safety and preliminary signs of efficacy in 18 previously untreated men with classic Fabry disease, a more severe disease form that manifests in childhood or adolescence.
Fabry Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Idorsia outlines new Phase 3 program for lucerastat in Fabry disease
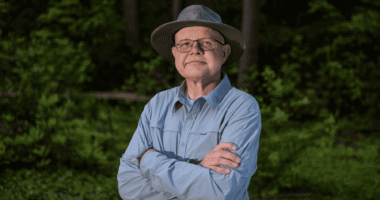
- Jeff’s Journey With Fabry Disease
- Eye vessel abnormalities may signal heart disease in Fabry patients
- We need more oral Fabry disease treatment options that reduce pain
- AMT-191 shows promise, but safety concerns prompt dosing pause
- Guest Voice: Believe us when we say we’re having a bad day
- Sangamo starts FDA submission seeking approval of Fabry gene therapy
- Managing my hypertension has required some trial and error
- Long-term use of lucerastat may protect kidneys in Fabry: Trial data
- Seeking good news as symptom relief eludes my children